Estrogen is a steroid hormone that can be imbalanced in both men and women, either through overproduction, increased exposure, or reduced detoxification and elimination. Increased exposure and reduced detoxification are responsible for the vast majority of estrogen imbalances.
Apart from menstrual irregularities in women, typical symptoms of estrogen dominance include the following:
- Weight gain, usually around the hips, thighs, and midsection
- Fibrocystic breasts in women and gynecomastia (male breasts) in men
- Fatigue
- Low libido
- Mood changes; for example, depression, anxiety, and/or irritability
To maintain healthy ratios of estrogen in women or minimize it in men, it's important to consider the influence that stress, the liver, and gut health have on estrogen clearance.
Stress and Catechol-O-methyltransferase
Catechol-O-methyltransferase, or COMT, is a gene that encodes for the enzyme that metabolizes catecholamines, including stress hormones like norepinephrine and epinephrine (cortisol) and estrogen. The COMT enzyme may work really well in some people, who are able to metabolize stress hormones and estrogen effectively, but it may be slower in others.

Stress can come from many sources, including the following:
- Emotional stress; for example, in family relationships, personal relationships, or work relationships
- Physical stress; for example, from overtraining or not sleeping enough
The COMT enzyme functions like a door. The door may be wide or narrow depending on a variety of factors, such as nutritional intake or genetic polymorphisms of the COMT gene that are being expressed. The stress hormones and estrogen have to pass through this COMT door in order to be metabolized, or broken down. If your door is narrow, it may limit the amount of stress hormones and estrogen that can pass through at the same time. If stress is low and estrogen is balanced, it most likely won't be a problem and you may never experience any discernible symptoms.
However, if either of these is higher than normal on a continual basis, as seen with estrogen dominance and/or chronic stress, and if the door is indeed narrow, it may affect metabolism of the other. Chronic stress would increase the demand for COMT door space to be given to cortisol, which means that less estrogen can get through, potentially leading to a high-estrogen scenario independent of estrogen production inside the body. It happens simply because the estrogen is not being metabolized properly.
The reverse is also true. In the presence of higher estrogen, more estrogen is likely to take up space, which may slow the metabolism of stress hormones and contribute to symptoms such as anxiety or sleeping difficulties.
You can support COMT enzyme function and the metabolism of estrogen and stress hormones by taking simple nutrients such as taurine and magnesium, as well as adaptogenic herbs such as ashwagandha, rhodiola, and the various ginsengs.*
Progesterone
Stress hormones can also block progesterone receptors. Cortisol is seen as an anti-progestin as cortisol and progesterone have very similar molecular structures, with both being able to bind to progesterone receptors.[1,2] The more cortisol binds to progesterone receptors, the fewer receptor sites are available for progesterone docking. A woman's body could register this as not having enough progesterone, even in the presence of normal progesterone levels.[3]
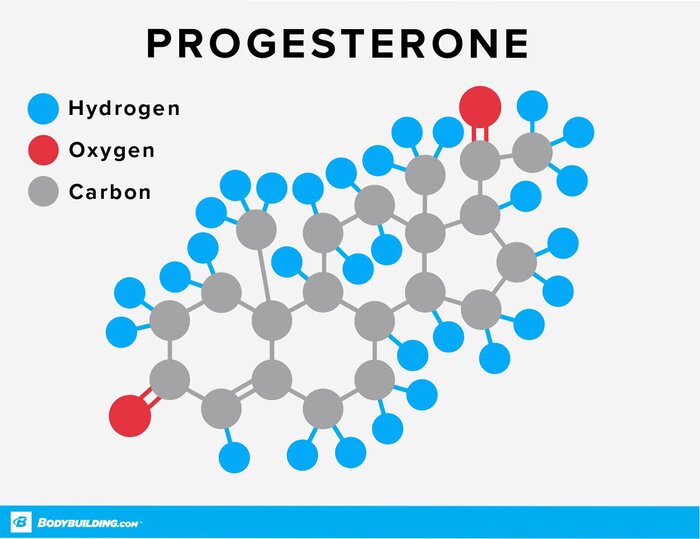
A lower progesterone-to-estrogen ratio may produce symptoms of estrogen dominance even in the presence of normal estrogen levels.
Estrogen
Everyone is exposed to estrogens. Men produce a small amount of estrogen in the testes and adrenal glands, while women produce a larger amount of estrogen in the ovaries and after menopause in the adrenal glands.
Both men and women will have higher estrogen levels in the presence of high body fat, since fat cells make estrogen. They can also be exposed to xenoestrogens via environmental sources such as plastics, pesticides, chemicals, and the water supply. Xenoestrogens are foreign estrogens but are close in molecular structure to natural estrogen, enabling them to bind to estrogen receptors and produce symptoms. To minimize exposure to xenoestrogens, reconsider your use of plastic water bottles, plastic protein shakers, and plastic lids on takeout coffee cups, especially in the presence of heat. Consider using glass or stainless-steel options instead. Removing the plastic lids from takeout cups before drinking is another good idea.

Leaky Gut
Chronic stress exposure can also contribute to gut dysbiosis and create imbalances between beneficial and less beneficial bacteria in the digestive system. There are a few reasons for this:
- Reduced secretory IgA antibodies in the gut mucosal wall. These are the first line of defense from the immune system. Low sIgA may delay an effective immune response and allow potential invaders to colonize the gut wall.
- Imbalances in other biochemical pathways, such as methylation. This can affect the formation of phospholipids, healthy bile production, and the ability of cells to repair.
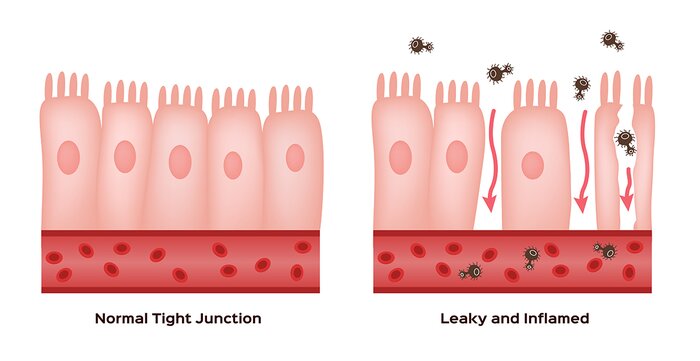
The resulting consequences can include leaky gut, gut dysbiosis, small intestinal bacterial overgrowth, food intolerances, and impaired estrogen detoxification, which can lead to estrogen dominance, weight gain, or both.
Estrobolome
This brings us to the all-important estrobolome. Many people are familiar with the microbiome, which refers to the collection of bacteria inside the digestive system (gut microbiome), the mouth (oral microbiome), and on the skin (skin microbiome). The species of bacteria in all these areas are not necessarily the same; some species are more dominant than others in specific areas, while other species are completely absent.
The estrobolome, on the other hand, is a collection of intestinal bacterial genes that metabolize and modulate estrogen in the gut.[4] It's a very important function of the estrobolome, as estrogen, like all other hormones and neuropeptides, is designed to be used, metabolized, and then eliminated through urine or feces. They are not meant to re-circulate inside the human body.
Estrogen Detoxification
Estrogen detoxification occurs during two main stages:
Stage 1
Estrogen detoxification starts in the liver via CYP450 enzymes and then occurs through processes such as methylation, sulfonation, and glucuronidation, in which estrogen metabolites are bound to other molecules, rendering them harmless. The COMT enzyme referred to above is responsible for the methylation of estrogen. Nutrients that are needed in Stage 1 include B vitamins, selenium, taurine, glycine, magnesium, and iodine.
Herbs such as rosemary promote normal hormone balance and support natural estrogen metabolism, as do broccoli, kale, and other cruciferous vegetables. Iodine, a mineral commonly found in seaweeds such as kelp, also supports natural estrogen metabolism.[5]

The conjugated estrogen metabolites formed from liver metabolism are then made water-soluble, allowing them to be excreted through the kidneys in urine. Alternatively, they can leave the liver through bile dumped into the small intestine in response to fat in the diet. What happens there depends largely on the estrobolome, which is Stage 2.
Stage 2
Some estrobolome bacterial species encode for enzymes such as beta-glucuronidase and beta-glucosidase, which can unbind estrogen that's destined for elimination through feces. This frees up harmful estrogen metabolites, allowing them to be reabsorbed back into circulation. All that estrogen that was supposed to leave the body is now back in circulation, contributing to symptoms of estrogen dominance.
Some common estrobolome bacteria that can reverse estrogen detoxification via this mechanism include species such as Clostridium, Citrobacter, Streptococcus and Klebsiella.[6]
Gut Microbial Richness
Gut microbial richness is determined by the number of bacterial genes in the digestive system, with a highly diverse gut microbiome having increased richness and a higher gene count. Simply put, the more different species of bacteria you have, the more diverse your gut microbiome and, as a result, the more bacterial genes are present that can detoxify estrogen. On the other hand, the lesser the diversity, the more likely you are to have greater numbers of bacterial species that contain beta-glucuronidase and beta-glucosidase enzymes, which have the potential for reversing estrogen detoxification.
Gut diversity is negatively affected by these factors:
- Excessive alcohol use
- Antibiotics (from food as well as prescriptive)
- Xenobiotics
- Pollutants
- Glyphosate exposure from nonorganic food
- A low-polyphenol diet, low in fruits and vegetables
Dietary polyphenols are found in the skins and peels of many colorful fruits and vegetables, as well as some grains such as black rice. Polyphenols have modbiotic properties, whereby they rebalance an unbalanced gut microflora and increase microbial diversity. Polyphenols can be metabolized by healthy gut bacteria such as Bifidobacterium spp. to produce the antimicrobial compounds needed to reduce more harmful or opportunistic species of bacteria.

Organic and seasonal sources of polyphenols are ideal, as these types of plant foods will contain greater amounts of polyphenols.
7 Ways to Optimize Your Estrogen Detoxification
To identify causes of estrogen imbalances, you need to assess estrogen in the body from the aspects of production (fat cells), exposure (xenoestrogens), and detoxification (liver, kidneys, and gut). Make changes where possible through better lifestyle choices, nutrition, exercise, and reduced alcohol intake.
Take steps to implement these seven strategies to improve your estrogen detoxification:
- Support adrenal function and balance or reduce your stress.
- Reduce inflammation.
- Support healthy kidney and liver function.
- Maintain healthy bile composition and release.
- Make sure that your bowels move regularly.
- Treat any gut dysbiosis.
- Increase microbial diversity.
References
- Karalis, Katia, et al. (1996). Cortisol blockade of progesterone: a possible molecular mechanism involved in the initiation of human labor. Nature Medicine, 2, 556-60.
- Leo, Joyce C. L., et al. (2004). Glucocorticoid and mineralocorticoid cross-talk with progesterone receptor to induce focal adhesion and growth inhibition in breast cancer cells. Endocrinology, 145(3), 1314-21.
- Holesh, Julie E., et al. (2020). Physiology, Ovulation. StatPearls Publishing.
- Plottel, Claudia S., & Blaser, Martin J. (2011). Microbiome and Malignancy. Cell Host Microbe, 10(4), 324-35.
- Stoddard, Frederick R., II, et al. (2008). Iodine alters gene expression in the MCF7 breast cancer cell line: evidence for an anti-estrogen effect of iodine. International Journal of Medical Sciences, 5(4), 189-96.
- Kwa, Maryann, et al. (2016). The intestinal microbiome and estrogen receptor-positive female breast cancer. Journal of the National Cancer Institute, 8(8), djw029.